Summary
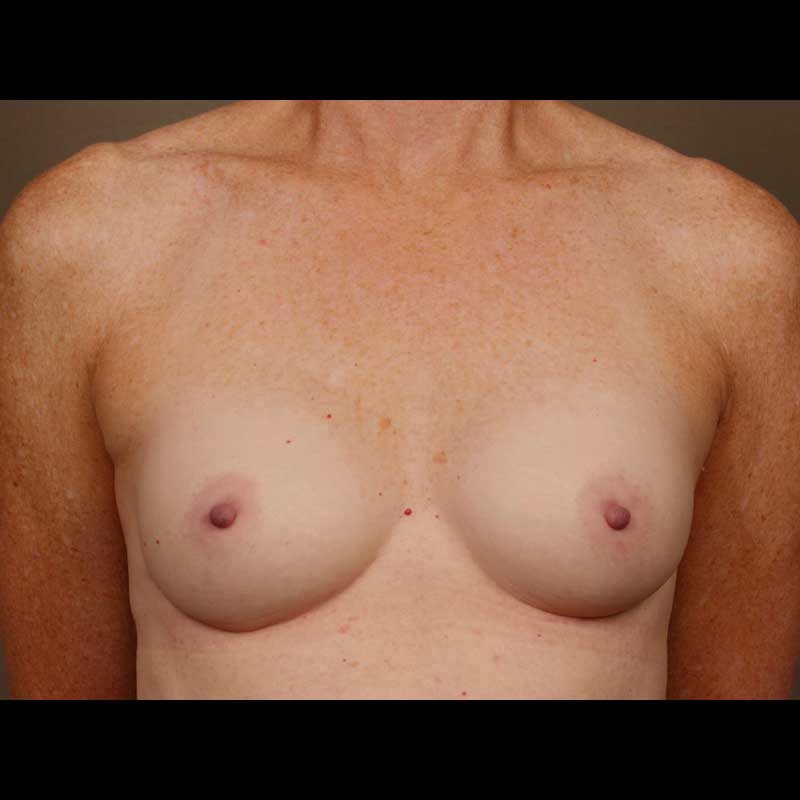
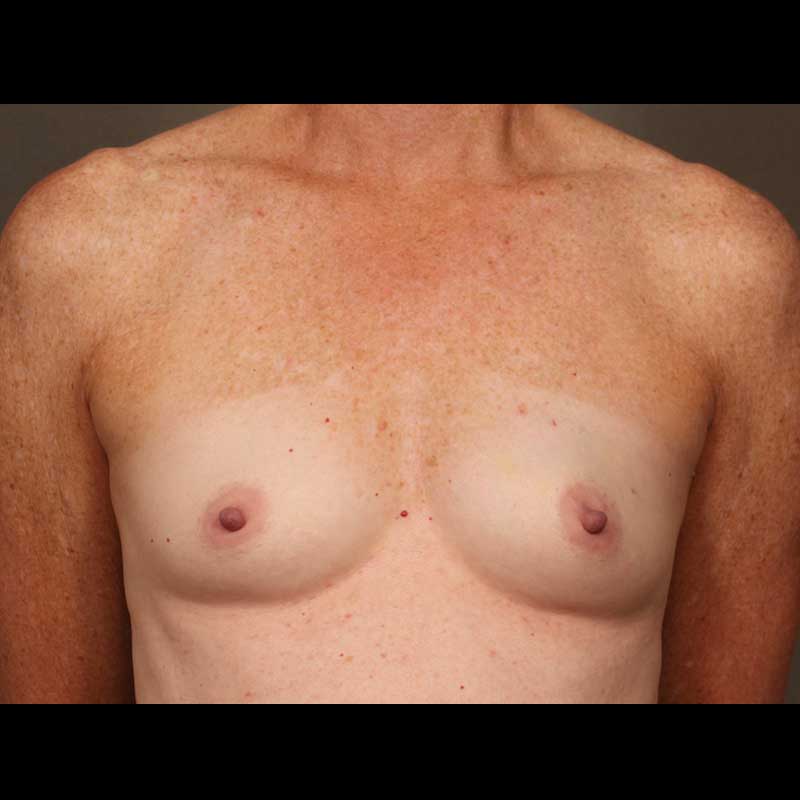
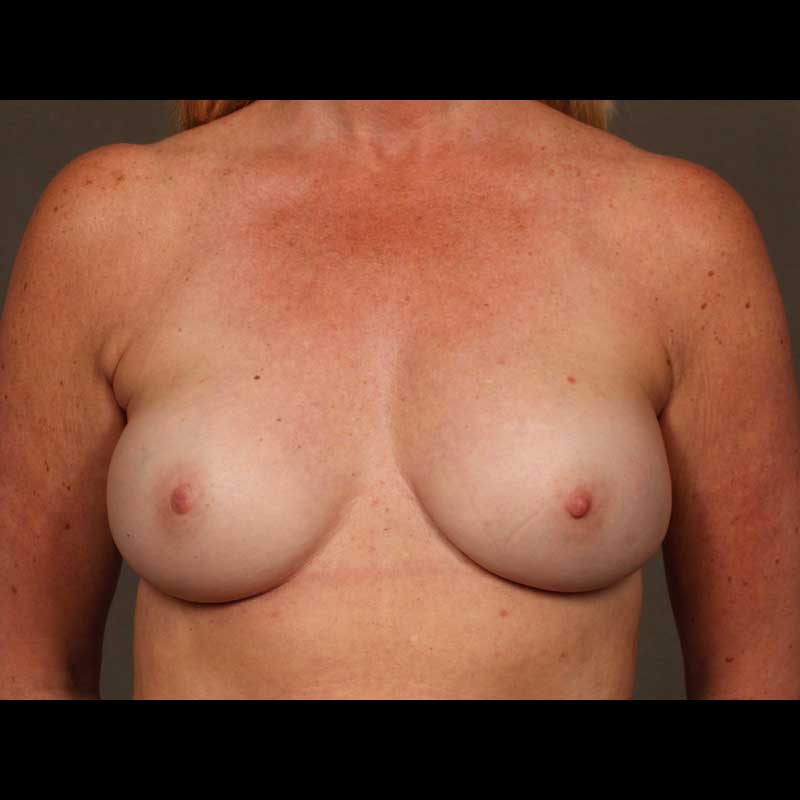
Direct-to-implant breast reconstruction can be a good option for patients with sufficient healthy breast skin following mastectomy. As skin-sparing and nipple-sparing mastectomy techniques continue to gain popularity, more and more women are good candidates for this “one-step” approach, which allows our surgeons to place a breast implant immediately, without using a tissue expander.
Types of procedures
- Prepectoral breast reconstruction: In the past, implants were always placed under the pectoralis muscle (UTM). Now, we can place the implants in a more natural position over the pectoralis muscle (OTM) in patients with good skin quality after mastectomy.
- Subpectoral breast reconstruction: It is still necessary to place implants under the pectoralis muscle (UTM) for some mastectomy cases. This subpectoral implant position allows for additional soft tissue beneath reconstructed breast skin.
Procedure details
- The type of implant chosen depends on patient anatomy and desires
- Implants can be placed over or under the pectoralis muscle
- A biologic tissue matrix placed around the implant helps secure the implant position
- Patients awaken from their mastectomy with a well-defined breast shape
- We can perform minor revision procedures at a second stage to improve breast shape
Risks & Benefits
The main reason patients choose implant breast reconstruction is that is allows for a shorter early recovery period compared with natural-tissue reconstruction.
Potential problems include malposition and breast skin rippling related to the breast implant. Over time, the natural capsule that forms around a breast implant can become thickened, possibly resulting in firmness or capsular contracture. These implant related problems can usually be corrected with relatively minor outpatient revision procedures.
Implant reconstruction can be difficult for patients with a history of radiation. Risks are also higher in patients with obesity and in patients with a very large breast size.
The surgeons at NYBRA Plastic Surgery take every precaution to mitigate these risks. We may suggest other options for breast reconstruction, including natural-tissue flaps, for patients who are not good candidates for implant reconstruction. In some cases, implants can be combined with flaps to provide a natural-looking breast reconstruction.
Frequently Asked Questions
How is the type of breast implant chosen?
After a comprehensive evaluation with one of our surgeons, including a detailed discussion concerning goals and desires, we help each patient determine the right implant shape, size, and type to fit their needs.
What is the difference between silicone gel implants and saline implants?
Both saline and silicone implants are approved by the FDA and can provide high quality breast reconstruction. The difference is that one type of implant is filled with saline and the other type is filled with silicone gel. Most patients choose silicone breast implants, which tend to be softer, potentially providing a more natural look and feel. Some women prefer saline implants, though they may be more prone to skin rippling.
How long do breast implants last before they need to be changed?
Breast implants do not need to be removed or changed unless a problem develops over time. While it is uncommon, if there is a leak in the outer shell of an implant, then the implant should be changed. If a saline implant has a leak, the implant volume deflates, making it relatively easy to diagnose. A silicone implant leak might require a breast MRI to be diagnosed. Leaky or otherwise problematic implants can be changed as an outpatient procedure without a difficult recovery.
Does insurance cover breast implants for breast reconstruction?
Yes. Federal guidelines based on the 1998 Women’s Health Care Rights Act mandate that insurance companies provide coverage for breast reconstruction. Any operation on the breast, including any type of breast plastic surgery, is covered by insurance for patients diagnosed with breast cancer. All stages of breast reconstruction are covered for patients undergoing mastectomies, including risk-reducing mastectomies.