Summary
Genetic mutations can occur naturally in the body. While some have no effect, other mutations can negatively impact health by increasing a person’s risk of developing cancer. Two genes in which harmful mutations have been shown to preferentially increase the risk of breast and ovarian cancer are known as the BRCA1 and BRCA2 genes. While BRCA1 and BRCA2 genes are the most well-known genes in which mutations can predispose to breast cancer, there are a number of other genes in which genetic mutations increase the risk of breast cancer. These include mutations in ATM, CHEK2, PALB2, PTEN, and TP53 genes, among others.
BRCA1 and BRCA2 genetic mutations
All people have the BRCA1 and BRCA2 genes, which normally function to help repair damaged breast cells. When these genes have harmful mutations, they don’t function normally, and the risk of developing breast cancer is higher. The presence of these gene mutations, which are passed on from one generation to the next, can be determined through a simple blood test. While the presence of harmful BRCA1 or BRCA2 gene mutations does not necessarily guarantee that breast cancer will develop (just as the absence of harmful BRCA1 or BRCA2 gene mutations does not guarantee that cancer will not develop), the risk of developing breast cancer is greatly increased among those who carry the mutations. It has been reported to be in the range of 55 to 65 percent for BRCA1 carriers and 45 to 55 percent for BRCA2 carriers.
Risk factors and genetic testing
There are a number of risk factors that are associated with the harmful gene mutations that are associated with breast cancer. These include having family members who have tested positive for these gene mutations, a family history of early onset breast cancer or ovarian cancer, early onset breast cancer yourself (in cases where cancer has already been diagnosed), and Eastern European or Ashkenazi Jewish ancestry. If you have any of these or other risk factors, the presence of harmful gene mutations can be determined through genetic testing. A genetic counselor can help guide you regarding your risks.
If you have a harmful genetic mutation, your breast surgeon and oncologist can help direct your treatment options. These include the use of risk-lowering medications, such as Tamoxifen and raloxifene, both of which may reduce the risk of developing estrogen-receptor positive breast cancers. A more definitive option is risk-reducing mastectomy. Most women who choose risk-reducing mastectomy also choose to have immediate breast reconstruction.
Types of procedures
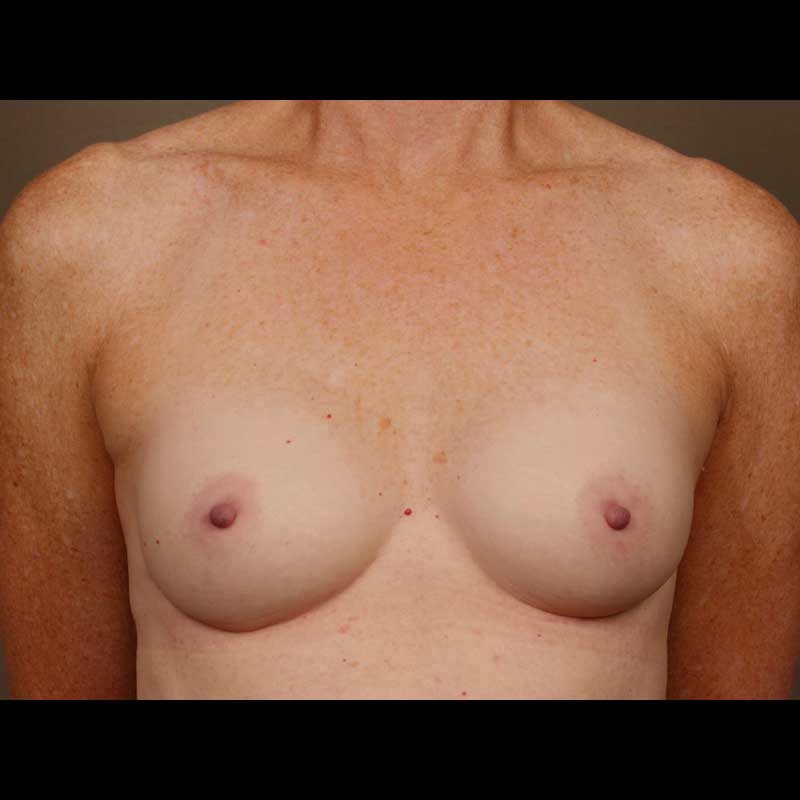
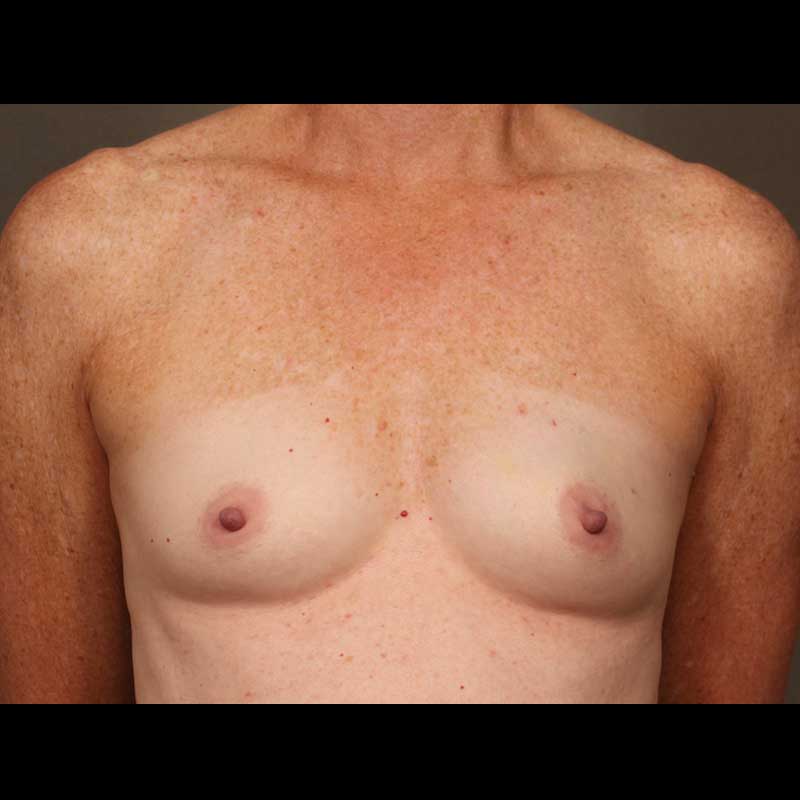
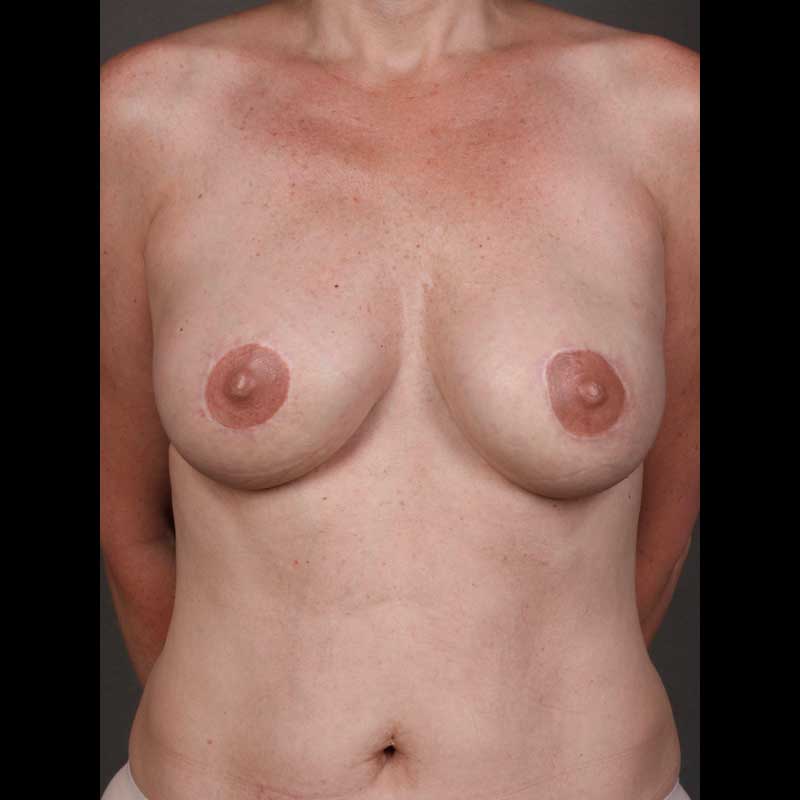
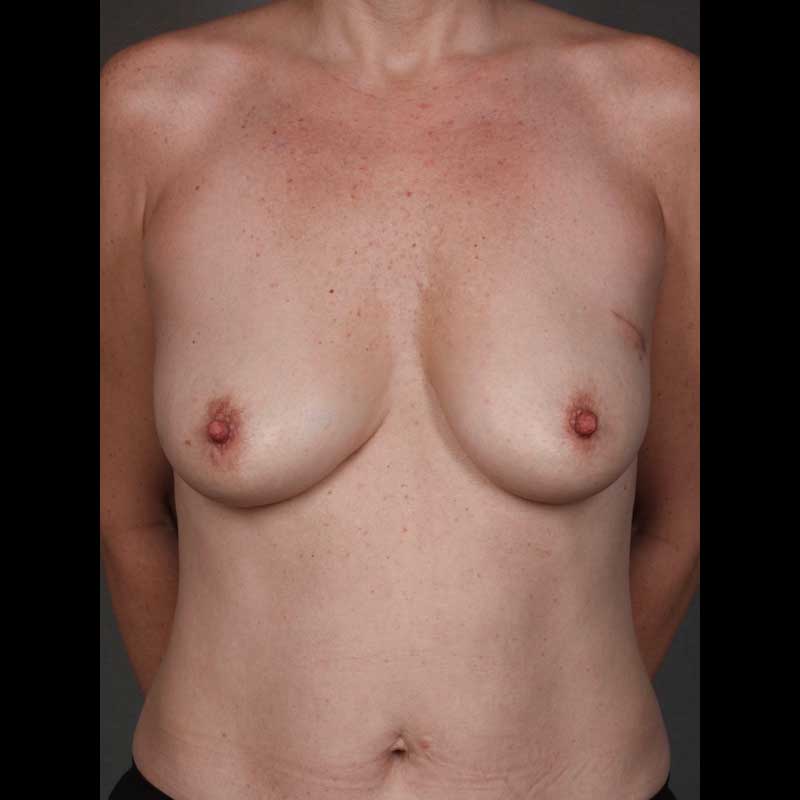
- Bilateral Risk-reducing Mastectomy: If you have an inherited genetic mutation that increases your risk of breast cancer, this surgery will dramatically reduce that risk. In most cases, the nipple and areola can be preserved, and the surgery can be planned with immediate breast reconstruction.
- Contralateral Risk-reducing Mastectomy: Women with a harmful genetic mutation who also have breast cancer can have a risk-reducing mastectomy to remove the opposite healthy breast at the same time as their cancer surgery. In most cases, this can be coordinated with immediate breast reconstruction.
Procedure details
- Evaluation with a genetic counselor can help you determine your risks
- Researchers have learned about moderate-risk and high-risk genetic mutations
- Multiple genetic mutations are now included with multi-gene testing (expanded panel testing)
- Your doctor can arrange for the blood test and have a detailed discussion with you about your risks and the potential benefits of testing
- If you find that you have a harmful genetic mutation, your breast surgeon and oncologist can help you make a decision about risk-reducing mastectomy
- You can decide to have bilateral skin-sparing mastectomy, where the nipple is removed, or you can choose bilateral nipple-sparing mastectomy
- Either way, the decision for bilateral risk-reducing mastectomy can be eased when you understand your options for breast reconstruction
- Breast reconstruction can be accomplished in one procedure coordinated with your breast surgeon
Risks & Benefits
Women decide to have risk-reducing surgery to ease their fear of breast cancer. By proceeding with surgery, they can feel that they have taken control and done everything possible to decrease their risk of getting breast cancer. This is particularly true for younger women found to have harmful genetic mutations.
The emotional impact of mastectomy can be diminished by knowing that breast reconstruction options are available. It is very important to understand your options for breast reconstruction early in the process. This can help guide your decisions about the choice and timing of risk-reducing mastectomy. The team at NYBRA Plastic Surgery is dedicated to helping you through the process from diagnosis to surgery and recovery.
Frequently Asked Questions
I think I am at high risk of getting breast cancer. Will insurance cover genetic testing?
If you meet criteria that place you in a high risk category, insurance should provide coverage for genetic testing. This can depend on the insurance company. Your breast surgeon or oncologist can help you with insurance authorization.
Will insurance cover risk-reducing mastectomy and breast reconstruction if I have a genetic mutation that puts me at high risk of breast cancer?
Unfortunately, there is no federal law that requires insurance companies to provide coverage for risk-reducing mastectomy if you don’t have cancer. In New York State, we have legal guidelines that require insurance companies to follow medical criteria, which are supported by medical literature. In our experience, if you have a harmful genetic mutation that is known to increase the risk of breast cancer, your insurance company will cover your surgery. If you undergo risk-reducing mastectomy for genetic mutation, the Women’s Health and Cancer Rights Act of 1998 is a federal law that requires insurance companies to provide coverage for breast reconstruction.