ERAS: A Thoughtful Approach to Post-Operative Pain Management
June 16, 2021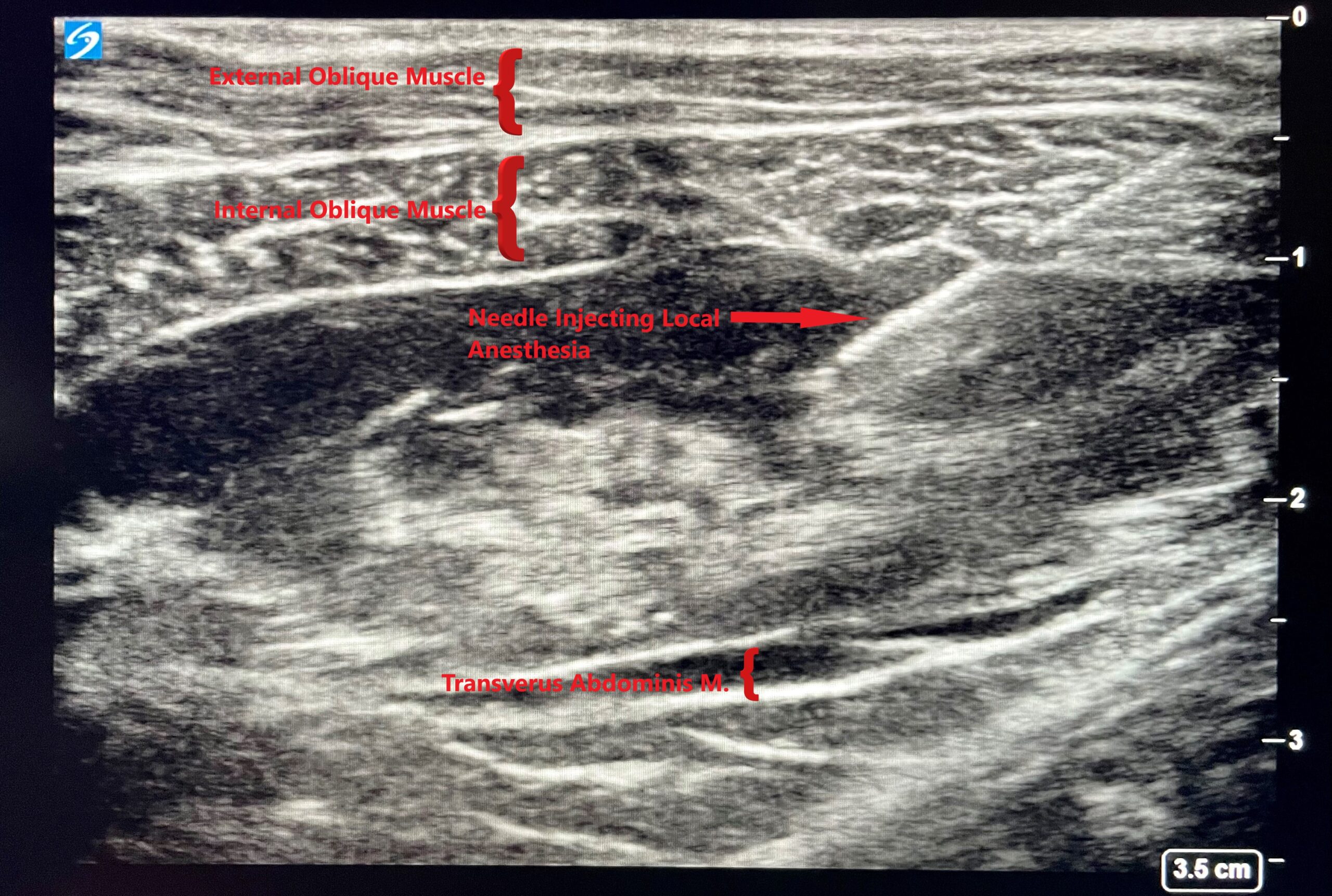
Postoperative pain management is an essential component of any successful procedure. Unfortunately, efforts to keep patients comfortable after surgery can sometimes be shortsighted, leaning on narcotic medications without considering their impact on overall health and recovery.
While it’s important to minimize discomfort, it’s equally important to do so in a way that considers the patient as a whole, along with both the long and short term impacts of treatment. Over the past several years, I’ve worked with our practice and the surrounding medical community to implement Enhanced Recovery After Surgery (ERAS) protocols. This approach has shortened hospital stays and dramatically improved comfort in our patients.
Read on to learn more about pain management strategies and how ERAS works.
PCA pumps can slow patient recovery.
When I was in training, it was common practice for patients to receive PCA (Patient Controlled Anesthesia) pumps filled with IV narcotic pain medication that they could deliver to themselves. This effort to ensure that patients did not need to wait for pain relief was admirable, however most patients did not need a lot of narcotic pain medication to remain comfortable after surgery. PCA pumps often left patients over-medicated and vulnerable to the many side effects of narcotic use, including itchy skin, drowsiness, nausea, vomiting, and painful constipation—just to name a few.
At that time, it was also common for patients to spend four days in the hospital following a DIEP flap or other autologous flap breast reconstruction. That additional time often had less to do with surgical recovery than it did the negative effects of narcotic pain medications, which were severe enough to prevent patients from getting out of bed and feeling better.
ERAS started as a plan for colorectal surgery patients.
In 2005, the first Enhance Recovery After Surgery (ERAS) protocol was published for colorectal surgery. This protocol stopped relying on IV narcotic medications for pain control in favor of a strategic multimodal approach with the goal of minimizing or eliminating narcotic pain medication. Since then, it has been adopted by many surgical specialties, including Plastic Surgery.
Our practice has been using a modified ERAS since 2014
In 2014, I began to employ a modified form of the ERAS protocol for my breast reconstruction patients. I immediately saw a difference in comfort and recovery. Over the last 5 years, I’ve given numerous lectures on the benefits of ERAS protocols and have successfully introduced an ERAS protocol for breast reconstruction in a number of hospitals, including St. Francis, St. Catherine’s, Mercy, Huntington, NYU Langone-Long Island and Mt. Sinai South Nassau Hospitals.
Pain management begins before surgery.
We work with our patients to optimize their condition before surgery by controlling or limiting risk factors associated with poor outcomes, including smoking, obesity, diabetes and alcohol consumption. On the morning of surgery, patients receive tylenol and NSAIDs (similar to ibuprofen).
Consistent monitoring is key.
Our team closely monitors every element of care throughout surgery, including the type of anesthesia provided, IV fluids, and body temperature. Patients also receive nerve blocks using long acting local anesthesia, which are an excellent way to control pain without narcotics. These include ultrasound guided TAP blocks in the abdomen and additional blocks in the breast.
ERAS protocols have most patients up and about within a day of surgery.
Patients receive Tylenol and IV NSAIDs for the first twenty-four hours following surgery. After twenty-four hours, they transition to oral tylenol and NSAIDs. Narcotic pain medication is provided for breakthrough pain, only if needed. A diet is resumed after surgery, and patients are out of bed and walking in less than 24 hours.
Through careful ERAS protocol implementation and patient education, we have been able to allow patients to return home comfortably in just 2 days. This approach has also significantly reduced and, in some cases, even eliminated postoperative narcotic pain medication use for our patients. Without the side effects associated with those medications, patients are more comfortable, out of bed sooner and eager to get back to the comforts of their own homes in less time. Recovery is about more than pain relief; it’s about getting well again. ERAS protocols remove one more barrier to restoration, so our patients can return to their lives that much quicker.
Easier Information Access with Outcomes4Me
A breast cancer diagnosis can be challenging to digest. Patients receive vast amounts of new information at once, which makes it hard to make choices…
